Table of Contents
Leprosy in India Today | NLEP | UPSC – IAS | The Hindu
National leprosy Eradication Programme
Initial reports of Leprosy Case Detection Campaign of the National Leprosy Eradication Programme (NLEP) indicated an all-time high of nearly 50,000 new leprosy cases in Bihar.
Today’s scenario 2019
- India was officially declared to have eliminated leprosy in 2005 when new cases fell to less than 1 per 10,000, yet India still accounts for the largest number of leprosy affected people in the world (58 per cent).
- Indian research contributed to the development of Multi-Drug Therapy or MDT, now recommended by WHO, which led to the shortening of treatment and higher cure rates.
- In recent years, along with other countries, India has repealed legislation that discriminates against persons affected by leprosy.
- In 2016, it repealed the draconian colonial-era Lepers Act and in January 2019 Lok Sabha passed a bill seeking to remove leprosy as a ground for divorce
What is Leprosy? | UPSC – IAS
- Leprosy is a chronic infectious disease caused by Mycobacterium leprae and is highly contagious.
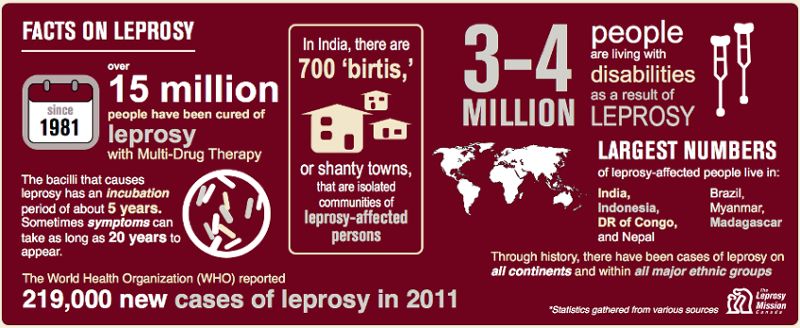
- The bacteria has a long incubation period. Once a person is infected, it can take 6-10 years or even 20 years for the first symptoms to surface.
- The disease mainly affects the skin, the peripheral nerves, the mucosa of the upper respiratory tract and the eyes.
- It is curable and treatment provided in the early stages averts disability. Mycobacterium Indicus Pranii (MIP)
- It is an indigenous vaccine for leprosy developed by National Institute of Immunology.
- It is now being introduced into the National Leprosy Elimination Programme (NLEP).
- It will boost the immune system against the bacterial disease.
Challenges in eradicating leprosy | UPSC – IAS | The Hindu
- Antimicrobial resistance in leprosy: Global data shows that a total of 8% of the Mycobacterium leprae bacterial strains studied showed gene mutations conferring resistance towards drugs such as rifampicin, dapsone and ofloxacin.
- Non-adherence to drugs: Due to various reasons a significant number of patients become irregular and default from MDT.
- Issues with 2005 declaration of Leprosy elimination:
- It led to the diversion of focus as both funding as well as resources declined and the frontline workers stopped making household visits to identify undetected cases, shifting instead to voluntary patient registration.
- The dermatologists didn’t send patients for treatment, as the strong rhetoric of elimination made them believe leprosy is a disease of the past.
- Neither funders nor young researchers are attracted to an officially eliminated disease, even if it is still ubiquitous.
- Stigma about leprosy: Fear of stigma, and the resulting discrimination, discourages individuals and their families from seeking the help they need.
- Lack of funding: Financial crunch in leprosy research and awareness campaigns leads to a shortfall in human reserves and trained medical professionals who can diagnose the disease correctly in its nascent stage.
Measures taken to eradicate Leprosy|UPSC – IAS | The Hindu
International Efforts
- Multidrug therapy, made available by WHO free of charge to all patients worldwide since 1995, provides a simple yet highly effective cure for all types of leprosy.
- In 2016, WHO launched The Global Leprosy Strategy 2016–2020: accelerating towards a leprosy-free world which aims to reinvigorate leprosy control efforts and avert disabilities, especially among children affected by the disease in endemic countries.
Government of India Initiatives (Govt Schemes for leprosy) | UPSC – IAS
- National Health Mission aims to reduce prevalence of Leprosy to <1/10000 population and incidence to zero in all districts.
- Ayushman Bharat’s 1,50,000 Health and Wellness Centres across the country plan to screen all Indians for leprosy.
- Sparsh Leprosy Awareness Campaign aims at communicating the importance of early detection and treatment of leprosy.
- New preventive approaches like chemoprophylaxis and immunoprophylaxis are being considered to prevent transmission.
- 30th of January (Martyrdom Day of Mahatma Gandhi) was celebrated all over India as Anti Leprosy Day to spread public awareness about the disease.
- A Leprosy Case Detection Campaign was launched in 2016, involving house-to-house screening and referral of patients for diagnosis.
- 12th Five year plan had set out to achieve elimination of leprosy at the district level by 2017.
India’s National Leprosy Eradication Programme | UPSC – IAS
It is a centrally sponsored Health Scheme of the Ministry of Health and Family Welfare which aims to eradicate leprosy from India.
Strategies for Leprosy Elimination
- Decentralized integrated leprosy services through General Health Care system.
- Early detection & complete treatment of new leprosy cases.
- Carrying out house hold contact survey in detection of Multibacillary (MB) & child cases.
- Early diagnosis & prompt MDT, through routine and special efforts
- Involvement of Accredited Social Health Activists (ASHAs) in the detection & complete treatment of Leprosy cases for leprosy work
- Strengthening of Disability Prevention & Medical Rehabilitation (DPMR) services.
- Information, Education & Communication (IEC) activities in the community to improve self-reporting to Primary Health Centre (PHC) and reduction of stigma.
- Intensive monitoring and supervision at Primary Health Centre/Community Health Centre.
A Way forward | UPSC – IAS | PCS
- Avoid shallow declarations: India remains a long way away from elimination at the state or district levels, let alone eradication. It is necessary to learn lessons and avoid creating an environment of complacency.
- Speedy implementation of the Health and Wellness Centres (HWC) initiative in the true spirit of comprehensive primary healthcare approach.
- Enhancing training of health-care providers: in communication and behaviour change skills, and by improving the patients’ access to quality care and friendly services.
- Adherence to MDT: can be improved by multiple initiatives that target the views and actions of patients, health-care workers, and society.
- Removal of stigma: Leprosy program managers should design positive health messages and use innovative media to appeal to and reach target groups to motivate leprosy patients to seek early treatment and the community to accept leprosy patients.
- Creating Livelihood Opportunities: Those who have been cured at an early stage and can work, should be given opportunities to learn skills and trades that would enable them to work.