Table of Contents
Malnutrition in India its types, causes and effects | UPSC – IAS
Malnutrition is a term that refers to any deficiency, excess or imbalance in somebody’s intake of energy and/or nutrients. It can either be due to inadequate intake or an excess intake of calories. The term malnutrition covers two broad groups of conditions are as follows:-
- Undernutrition – This includes stunting (low height for age), wasting (low weight for height), underweight (low weight for age) and micronutrient deficiencies or insufficiencies (a lack of important vitamins and minerals)
- Overnutrition – This includes overweight, obesity and diet-related non-communicable diseases (such as cardiovascular disease, hypertension, cancer, and type-2 diabetes.).
Types of Malnutrition | UPSC – IAS
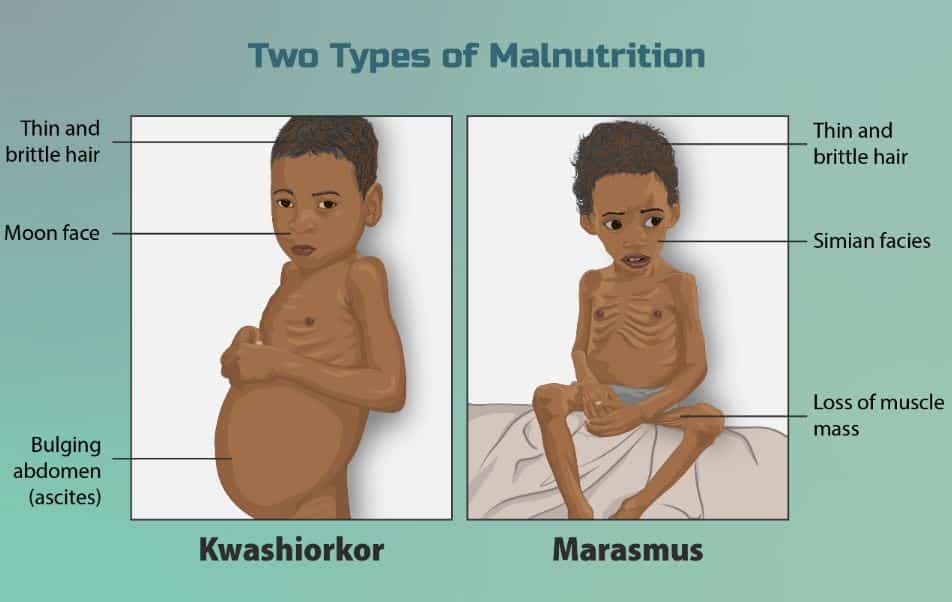
- Marasmus – It is a form of severe malnutrition. Nutrient deficiency is the main cause of marasmus. It occurs in children that don’t ingest enough protein, calories, carbohydrates, and other important nutrients. This is usually due to poverty and a scarcity of food.
- Kwashiorkor – It is a form of severe protein malnutrition. In this type malnutrition produced by a severely inadequate amount of protein in the diet.
Fundamental Causes behind Malnutrition in India | UPSC – IAS
The causes and consequences of malnutrition are complex, and it will require the concerted efforts of all social institutions, including the social work profession, to combat malnutrition effectively.
- Barriers to health services include – High cost of care. Inadequate or no insurance coverage. Lack of availability of services.
- Poverty – It hinders the accessibility of adequate food. (Poverty is the single most common cause of food insecurity)
- Social strains on Women – Early marriages of girls leads to teenage pregnancies resulting in low birth weight of the newborns, poor breastfeeding practices and poor complementary feeding practices.
- Lack of availability of safe drinking water hinders proper digestion and assimilation of food and also cause water and food borne diseases.
- Poor sanitation – It is linked to transmission of diseases such as cholera, diarrhoea, dysentery, hepatitis A, typhoid and polio and exacerbate stunting. It reduces human well-being, social and economic development. Poor sanitation and environmental conditions lead to spread of many diseases that sap children’s energy and stunts their growth.
- illiteracy in women and large household size.
- Lack of Awareness: about nutritional needs of infants and young children.
Malnutrition In India | UPSC – IAS
Despite India’s 50 percent increase in GDP since year 2013, more than one third of the world’s malnourished children live in India. Among these, half of the children under 3 years old are underweight.
- An approximate 23.6% of the population of India live below a purchasing power of 92 INR a day. This poverty does not directly lead to malnutrition but it leaves a large piece of the population without sufficient amounts of food.
The World Bank (WB) estimates that India is one of the highest-ranking countries in the whole world for the number of children suffering from malnutrition. The prevalence of underweight children in India is among the highest in the world and is nearly double that of Sub Saharan Africa with dire consequences for mobility, mortality, productivity, and economic growth.
- One of the major causes for malnutrition in India is economic inequality. On account of the low social status of the population, their diet often lacks in both quality and quantity. Mostly Women who suffer from malnutrition are less likely to have healthy babies.
- Nutrition deficiencies inflict long-term damage to both individuals and society. Compared with their better-fed peers, nutrition-deficient individuals are more likely to have infectious diseases such as pneumonia and tuberculosis, which lead to a higher mortality rate.
Effects of Malnutrition in India | UPSC – IAS
Poverty increases the risk of, and risks from, malnutrition. Low income families are more likely to be affected by different forms of malnutrition. Moreover, malnutrition increases health care costs, reduces productivity & morale, and slows economic growth, which can perpetuate a cycle of poverty and ill-health.
- Increased vulnerability to diseases: Undernutrition increases the risk of infectious diseases like diarrhoea, measles, malaria and pneumonia.
- Developmental delays: Chronic malnutrition can impair a young child’s physical and mental development. Cognitive impairment resulting from malnutrition may result in diminished productivity in academic performance.
- Low productivity later in life: As per estimates of World Bank, childhood stunting may result in a loss of height among adults by 1%, which may further lead to a reduction in individuals economic productivity by 1.4%
- Poor maternity health: Undernutrition puts women at a greater risk of pregnancy-related complications and death (obstructed labour and hemorrhage).
- Barrier to socio-economic development: Widespread child undernutrition greatly impedes a country’s socioeconomic development and potential to reduce poverty.
Why malnutrition is a problem ? | UPSC – IAS
Underlying causes of malnutrition – The lack of money for food; and insufficiency of food production. It is stressed that much agricultural land is employed for purposes other than the production of food. Other causes of malnutrition include changes in local food habits and in food technology.
- Reduced household incomes: In recent years slowdown in economic growth, stagnant rural wages and high levels of unemployment have affected household incomes and limited their ability to invest in nutritional food.
- Underfunding: For instance, in a response to a parliamentary question in December 2019, the Minister for Women and Child Development presented data which showed that only about 32.5% of the funds released for Poshan Abhiyaan from 2017-18 onwards had been utilised.
- Poor implementation of schemes: Anganwadi centres were established under ICDS to provide basic healthcare education and services across the country. Many workers are unable to play an effective role in attending to the problem of malnutrition because of low wages and inadequate training.
- lack of access to safe water, sanitation and hygiene, ignorance and lack of education, social and cultural factors like child marriage, caste barriers etc.
Solution to the problem of malnutrition (In brief) – Increasing yields by organic manuring and mixed cropping; devoting more land to staple food production; changes in food habits and in food technology.
Steps taken by Government for nutritional well being | UPSC – IAS
- POSHAN Abhiyaan or National Nutrition Mission: It is Government of India’s flagship programme to improve nutritional outcomes for children, pregnant women and lactating mothers.
- Under it the Anemia Mukt Bharat (AMB) Strategy was launched in 2018 with efforts to improve Iron and Folic Acid (IFA) supplementation, behaviour change and anaemia-related care and treatment across six target groups including pregnant women, lactating mothers, and children.
- Integrated Child Development Scheme (ICDS): It aims to improve the nutritional and health status of children in the age-group 0-6 years and reduce the incidence of mortality, morbidity, malnutrition and school dropout.
- Public Distribution System: It provides coverage to upto 75% of rural population and upto 50% of urban population for receiving highly subsidized food grains under Targeted Public Distribution System.
- Midday meal scheme: The scheme provides meals for all school children studying in Classes I-VIII of Government, Government-Aided Schools.
Eradicating Hunger poverty and Malnutrition together in India | UPSC – IAS
In today’s world, eradicating hunger, food insecurity and all forms of malnutrition calls not only for reduced rural poverty and improved resilience of the most vulnerable people, but also for efficient food systems which are able to deliver sufficient and nutritious food for everyone. However, to make this happen, strong political commitment at global, regional and especially national levels is necessary.
To Enhance the effectiveness of the POSHAN Abhiyaan in India:-
- Implement POSHAN-plus strategy which apart from continued strengthening the four pillars (technology, convergence, behavioural change and capacity building) of the Abhiyaan also requires addressing the governance challenges of National Health Mission (NHM)/ ICDS delivery mechanism and renewed focus on
- Complementary feeding (usually targeted at the age range of 6-24 months)
- Investments in education of girls and women, reduce early marriage and early pregnancy, improving care during and after pregnancy etc.
- Availability of regional food items and cultural preferences may also be integrated with this abhiyaan to make it inclusive.
- Enhance the reach of the POSHAN Abhiyaan: Since the Anganwadi centres (AWCs) are at the heart of POSHAN Abhiyaan, it is imperative to enhance their reach. Therefore, mini Anganwadi centres should be set up so that children, pregnant and lactating women who may not be able to travel longer distances, have easier access to them.
- Institutionalise Capacity Building: Regular trainings for Anganwadi; availability of basic amenities such as electricity, growth monitors, supplies are imperative for proper functioning of the AWCs and the effective provision of services.
- Strengthen Coordination: All the programmes of the government having direct or indirect impact on the nutrition must be brought under the POSHAN Abhiyaan.
- Nurture Community Approach: Despite strong efforts, community involvement in POSHAN Abhiyaan has been substandard. State specific efforts should be made (keeping in view the diversity and intersectionality of the society) for ensuring community participation.
Conclusion and A way forward | UPSC – IAS
- Developing an employment-centred growth strategy: which includes universal provision of basic services for education, health, food and social security.
- Strengthening present initiatives: Direct interventions such as supplementary nutrition (of good quality including eggs, fruits, etc.), growth monitoring, and behaviour change communication through the ICDS and school meals must be strengthened and given more resources.
- Need of Data initiative: A modern data initiative leveraging and combining aspects of the NFHS, the National Nutrition Monitoring Bureau and the National Sample Surveys that collected data on detailed household-level consumption and expenditure on various food items should be considered.
- Improve dietary pattern by promoting production and increasing per capita availability of nutritionally rich food.
- Targeted approach: The government agencies in India need to adopt a comprehensive and coordinated multisectoral approach which is formulated by taking into account the varied nature of local-level challenges.
- Food fortification: A proposed policy would provide for adding essential vitamins and minerals (iron, folic acid, vitamin, iodine) to food items (rice, wheat flour, salt, edible oil, milk) sold in markets. The Centrally Sponsored Pilot Scheme on Fortification of Rice & its distribution through Public Distribution System is a step in the right direction.